Bruger:Christian89/Sandkasse2
| Christian89/Sandkasse2 Klassifikation | |
|---|---|
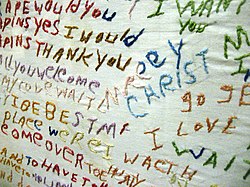 Tøj broderet af en person lidende af skizofreni. | |
| Information | |
| Navn | Christian89/Sandkasse2 |
| SKS | DF20 |
| ICD-10 | F20 |
| ICD-9 | 295 |
Skizofreni er en psykisk lidelse karakteriseret ved forstyrrelser i tankeprocesserne og hæmning af typisk følelsesmæssig reaktion.[1] Hyppigt sete symptomer inkluderer hørelseshallucinationer, paranoide og bizarre vrangforestillinger samt tanke og taleforstyrrelser, som oftest er associeret med nedsat social interaktion. Symptomerne på skizofreni debuterer oftest i teenageårene eller ung voksenalder med global livstidsprævalens på 0.3–0.7%.[2] Diagnosen er baseret på observationer af patientens opførsel og vedkommenes beskrivelse af sine oplevelser.
Skizofreni er afledt af græsk skhizein (σχίζειν, "spaltet") og phren (φρήν, φρεν-; sind), men der er ikke tale om personlighedsspaltning, som det oftest forveksles med i folkemunde.[3] Derimod henviser ordet til en spaltning af tanker og følelser.[4]
Nogle af de vigtigste faktorer der antages at være afgørende i udviklingen af skizofreni involverer genetik, tidlige miljømæssige påvirkninger, neurobiologi, psykosociale og sociale interaktioner. Nuværende forskning fokuserer især på neurobiologiske mekanismer, men der er endnu ikke blevet fundet nogen selvstændig organisk årsag. De mange forskellige symptomer har givet anledning til overvejelser om diagnosen repræsenterer en enkel lidelse eller flere forskellige syndromer.
Den primære behandling af skizofreni involverer antipsykotisk medicin, som hæmmer dopaminerg (og nogle gange serotonerg) receptoraktivitet. Psykoterapi og social genetablering er ligeledes vigtige led i behandlingen. I mere alvorlige tilfælde hvor vedkommende kan være til fare for sig selv eller sine omgivelser, kan tvangsindlæggelse være nødvendig. Disse tvunge hospitalsophold er dog af kortere varighed og mindre anvendte i dag.[5]
Personer med skizofreni lider oftest også af andre tilstande (co-morbiditet), som inkluderer depression og angst samt misbrugsproblemer.[6] Sociale problemer som langtidsarbejdsløshed, fattigdom og hjemløshed er oftest sete. Middellevetiden for mennesker med denne lidelse er 12 til 15 år mindre end dem uden, hvilket er et resultat af fysiske sundhedsproblemer og høj selvmordsrate (omkring 5%)[2][7]
Symptomer
redigérSkizofreni er karakteriseret ved problemer med tankeprocesserne, der kan lede til forstyrret tankeindhold (vrangforestillinger) og/eller tankeform (sproglige tankeforstyrrelser). Sidstnævnte symptom indebærer forstyrrelser i tankerne, som kommer til udtryk i sproget.[8] Eksempelvis kan disse vise sig som dannelse af nye ord (neolgismer), opløsning af sætningsstrukturen (inkohærens), associationsforstyrrelser hvor patientens tankegang følger et mønster, der er svært at sætte sig ind i for en udestående.[9] Ligeledes ses forstyrrelser af sanseoplevelserne i form af hallucinationer, (hvor hørelseshallucintaioner er den hyppigst sete form).[8]
De forstyrrede tankeprocesser kan også give andre kognitive symptomer, der omfatter problemer med arbejds- og langtidshukommelse, koncentrationsevne, hastigheden af informationsbearbejdning og eksekutivfunktioner (f.eks begrebsdannelse, ordmobilisering, evnen til at danne, fastholde og skifte kognitive strategier).[2]
Social kognition er også fundet nedsat, og menes at bidrage til adfærdsmæssige symptomer som social tilbagetrækning[10]. Udover social isolation[11] er hygiejneforsømmelse, tab af motivation og dømmekraft,[12] samt hæmmet emotionel reaktion[13] også ofte sete adfærdsmæssige symptomer. Mellem 30 og 50% lidende af skizofreni har ingen sygdomsindsigt.[14]
I visse tilfælde kan der også forekomme bevægelsesmæssige forstyrrelser i form af katatone symptomer, hvor patienten fastfryses i forvredne stillinger i længere tid.[15]
Schneideriansk klassifikation
redigérI begyndelsen af det 20. århundrede opstillede den tyske psykiater Kurt Schneider en række psykotiske symptomer, som han mente adskilte sig fra andre psykotiske lidelser. Disse kaldes førsterangssymptomer, og inkluderer styringsoplevelse (følelsen af at blive kontrolleret af en udefrakommende kraft), tankepåvirkningsoplevelse (følelsen af at ens tanker stjæles, påføres, kan høres eller overføres til omgivelserne), tredjepersons hørehallucinationer (høre kommenterende stemmer eller diskuterende stemmer)[16].
Selvom førsterangssymptomerne har været definerende for de diagnostiske kriterier for skizofreni, er disses specifitet omdiskuteret: I en oversigtsartikel baseret på diagnostiske studier indsamlet mellem 1970 og 2005 blev der hverken fundet be- eller afkræftelse på Schneiders opstilling, hvilket har ledt til forslaget om at førsterangssymptomer burde have mindre vægt i de kommende diagnose klassifikationssystemer. [17]
Positive og negative symptomer
redigérI klinikken skelnes der oftest mellem positive og negative symptomer.[18] De positive symptomer dækker over vrangforestillinger (ofte forfølgelses eller bizarrre forestillinger), tanke- og taleforstyrrelser samt hallucinationer som både kan påvirke føle-, hørelse-, syns-, lugte- og smagssanserne, som er typiske træk ved psykoser.[19] Hallucinationerne er ofte associeret med vrangforestillingernes indhold.[20] Den antipsykotiske medicin har meget gunstig effekt på de positive symptomer.[20]
Negative symptomer dækker over fravær af en række normale psykologiske og sociale funktioner, som den antipsykotiske medicin er mindre gavnlig overfor.[12] Disse indebærer typisk sløvhed, affektafladning, sprogfattigdom, manglende interesser, social tilbagetrækning og indsynken i sig selv.[21] Undersøgelser peger på at negative symptomer medfører dårligere livskvalitet, ringere fremdrift og større byrde for omgivelserne end de positive symptomer.[22] Individer med fremtrædende negative symptomer har hyppigt i forvejen dårlig tilpasningsevne inden sygdomsdebut og responderer også dårligere på medicinen.[12][23]
Sygdomsdebut
redigérDe sene teenageår samt tidlig voksenalder er en afgørende periode for udvikling af sociale og faglige kompentencer,[24] og er også den typiske periode for udvikling af skizofreni.[2] 40% af mændene og 23% af kvinderne diagnosticeret med skizofreni havde sygdomsdebut før 19 års alderen.[25] For at reducere udviklingsforstyrelserne associeret med skizofreni, er der blevet iværksat store undersøgelser med henblik på at identificere og behandle den prodrome (før-debut) fase af sygdommen, som er blevet observeret helt op til 30 måneder før det endelige sygdomsdebut.[24]
Individer i den prodrome fase kan opleve korte forbigående psykotiske symptomer[26] og ikke-specifikke symptomer som social tilbagetrækning, irritabilitet, kortvarig forstemt tristehed (dysfori)[27] og klodsethed[28]
Årsager
redigérEn kombination af genetiske og miljømæssige faktorer spiller en rolle for udviklingen af skizofreni.[2][3] Individer beslægtet med personer diagnosticeret med skizofreni som oplever en forbigående psykoser har 20-40% sandsynlighed for at få diagnosen er år senere.[29]
Genetik
redigérDer er stor variation i den estimerede familiære arvelighed af skizofreni, hvilket skyldes forskelle i diagnostik, statistiske forhold[30] samt vanskeligheder med at adskille genetiske og miljømæssige faktorer.[31] Til trods for den store variation i estimaterne er der dog blevet påvist en signifikant forhøjet risiko for udvikling af skizofreni i familier med sygdommen sammenlignet med raske kontrolgrupper.[30] Den største risiko for at udvikle skizofreni er at have førstegenerationsslægtninge med sygdommen (risiko på 6,5%). Ved forældre begge lidende af skizofreni stiger risikoen for at få et afkom med lidelsen til 46%.[32]
Tvillingestudier har anslået at mere end 40% af fuldkommen genetisk identiske enæggede tvillinger, med forældre lidende af skizofreni, får symptomer på lidelsen.[33] Den resterende procentdel angiver tilfælde, hvor kun en af tvillingerne eller ingen af tvillingerne har arvet sygdommen, hvilket indikerer også ikke-genetiske faktorer (som f.eks. miljø) er involveret.[32]
Molekylærgenetiske studier har ikke fundet noget specifik gen knyttet til skizofreni, men identificeret en række risikogener som menes at være involveret i udviklingen. Viden om hvor meget disse øger risikoen er dog begrænset,[34] og det menes at generne hver bidrager med en mindre effekt, som i kombination med miljømæssige faktorer kan overstige en hvis tærskelværdi, som leder til udtryk af symptomerne.[32] Riskogentiske kandidater involverer bla. ændringer i generne kodende for proteinerne neuregulin 1, dysbindin og catechol-O-methyltransferase, som menes at kunne lede til ændret funktion af disse og derved forstyrrelser i den synaptiske transmission mellem nervecellerne (som er en forstyrrelse karakteristisk for skizofreni).[35] Yderligere synes der at være et signifikant overlap mellem gener for skizofreni og bipolær affektiv sindslidelse.[36]
Fra evolutionspsykologisk perspektiv er der dog blevet fokuseret på hvorfor gener der øger tendensen til psykose er blevet nedarvet, da disse lidelser er uhensigtmæssige fra et evolutionært synspunkt. En påstand er at de samme gener som øger risikoen for psykose også er involveret i sprog og menneskelig adfærd, men disse påstande er til dato kun hypotetiske.[37][38]
Miljø
redigérMiljømæssige faktorer associeret med udviklingen af skizofreni inkluderer opvækstmiljøet, brug af visse euforiserende stoffer og graviditetskomplikationer som f.eks. lav fødselsvægt.[39] Opdragelse virker ikke til at have nogen betydelig indvirkning på udvikling af skizofreni, men det lader til at individer med støttende forældre bedre håndterer deres skizofreni end personer med bearbejdende og fjendtlige forældre.[3] Opvækst som barn og bopæl som voksen i storbyen er konsekvent blevet fundet at øge risikoen for udviklingen af skizofreni med en faktor to,[2][3] selv efter at have medregnet brug af euforiserende stoffer, etnicitet og størrelsen af ens sociale omgangskreds. Andre faktorer som spiller en vigtig rolle inkluderer social isolation, immigration associeret med social udstødelse, racistisk diskrimmination, dårligt fungerende familier, arbejdsløshed og dårlige boligtilstande.[3][40]
Brug af stoffer
redigérAmfetamin, kokain og til en mindre grad alkohol kan resultere i skizofrenilignende psykoser.[3][41] Der ses ligeledes et højere forbrug af nikotin blandt individer lidende af skizofreni sammenlignet med den generelle befolkning. Nikotin menes dog ikke at bidrage til udviklingen af lidelsen.[42] Misbrug blandt skizofrene er udbredt, og det anslås at over halvdelen indtager større mængder alkohol eller andre euforiserende stoffer.[43] Epidemiologiske studier har i de senere år belyst en relation mellem cannabismisbrug og tidligere debut af skizofreni - en association som ikke blev fundet ved alkoholmisbrug.[44] Brugen af stoffer menes ligeledes at fungerer som et værktøj til at håndtere andre omstændigheder blandt skizofrene som depression, angst, kedsomhed og ensomhed.[43][45]
Der er beviser på at alkoholmisbrug via en kindling mekanisme kan medføre udvikling af kronisk psykotiske tilstande som f.eks. skizofreni.[46] Epidemilogiske studier peger på, at jo oftere cannabis bruges jo større risiko er der for at udvikle en psykotisk tilstand.[47] For det enkelte individ menes hyppigt brug, at fordoble risikoen for udvikling af psykoser og skizofreni.[48] Der er dog stadig stor uenighed om det er cannabismisbrug som leder til udviklingen af skizofreni, eller cannabismisbrug er en adfærd knyttet til lidelsen.[49][50]
Fosterskader
redigérOmstændigheder som iltmangel, infektioner, stress og underernæring hos den gravide kan medføre udvikling af skizofreni ved afkommet senere i livet.[2] Individer diagnosticeret med lidelsen er ofte født om vinteren eller foråret, hvor der er størst risiko for virale infektioner af fosteret.[3] Mistanken om sammenhængen mellem underernæring og udvikling af skizofreni er bla. baseret på en periode under 2. verdenskrig, hvor vestlige dele af Holland var blokeret af tyskerene og der var udbredt sult, mens den østlige del ikke var så hårdt ramt. Sammenligning mellem de to grupper viste at fostre i vinteren 1944-1945 havde en øget risiko for senere at udvikle skizofreni som følge af den dårligere ernæring.[51]
Psykopatologi
redigérFlere neuropsykiatriske studier har forsøgt at forklare sammenhængen mellem ændret hjernefunktion og skizofreni, hvilket har ledt til en række fund og teorier.[52] En af de mest kendte er dopaminhypotesen, som antager at skizofreni skyldes øget dopaminerg signalering i hjernens pandelapper.[2]
Psykologisk
redigérHos et flertal af patienterne er der fundet ændringer i de kognitive funktioner.[53] Blandt individer diagnosticeret med skizofreni (eller med risiko for udvikling af lidelsen) er der blevet observeret kognitive biasser, især når disse er under stress eller i forvirrende situationer.[54] Andre kognitive ændringer involverer områder som hukommelse, opmærksomhed og eksekutivfunktioner, men kan også relateres til specifikke situationer eller oplevelser.[55][56] Mange af de kognitive forstyrrelse afspejles i de negative symptomer.[53]
Til trods for den ofte hæmmet følelsesmæssige reaktion viser nyere studier, at individer diagnosticeret med skizofreni er i stand til at reagere emotionelt, især på stressende eller negative stimuli, og at denne form for overfølsomhed kan give øget sårbarhed for symptomerne og lidelsen.[57][58] Visse fund tyder på at vrangforestillingernes indhold i en psykotisk episode kan afspejle emotionelle årsager, og hvordan en person tolker disse oplevelser kan have indflydelse på symptompatologien.[59][60][61] Tendensen til sikkerhedsadfærd overfor vrangforestillingernes indhold kan bidrage til varigheden af disse.[62] Yderligere beviser på de psykologiske mekanismers rolle kommer fra effekten af psykoterapi på symptomerne ved skizofreni.[63]
Neurological
redigérSchizophrenia is associated with subtle differences in brain structures, found in 40 to 50% of cases, and in brain chemistry during acute psychotic states.[2] Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus and temporal lobes.[64] Reductions in brain volume, smaller than those found in Alzheimer's disease, have been reported in areas of the frontal cortex and temporal lobes. It is uncertain whether these volumetric changes are progressive or preexist prior to the onset of the disease.[65] These differences have been linked to the neurocognitive deficits often associated with schizophrenia.[66] Because neural circuits are altered, it has alternatively been suggested that schizophrenia should be thought of as a collection of neurodevelopmental disorders.[67]
Particular attention has been paid to the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that phenothiazine drugs, which block dopamine function, could reduce psychotic symptoms. It is also supported by the fact that amphetamines, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia.[68] The influential dopamine hypothesis of schizophrenia proposed that excessive activation of D2 receptors was the cause of (the positive symptoms of) schizophrenia. Although postulated for about 20 years based on the D2 blockade effect common to all antipsychotics, it was not until the mid-1990s that PET and SPET imaging studies provided supporting evidence. The dopamine hypothesis is now thought to be simplistic, partly because newer antipsychotic medication (atypical antipsychotic medication) can be just as effective as older medication (typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect.[69]
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia, largely because of the abnormally low levels of glutamate receptors found in the postmortem brains of those diagnosed with schizophrenia,[70] and the discovery that glutamate-blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition.[71] Reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function, and glutamate can affect dopamine function, both of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in the condition.[72] But positive symptoms fail to respond to glutamatergic medication.[73]
Diagnosis
redigérSchizophrenia is diagnosed based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, version DSM-IV-TR, or the World Health Organization's International Statistical Classification of Diseases and Related Health Problems, the ICD-10.[2] These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by a clinical assessment by a mental health professional. Symptoms associated with schizophrenia occur along a continuum in the population and must reach a certain severity before a diagnosis is made.[3] As of 2009 there is no objective test.[2]
Criteria
redigérThe ICD-10 criteria are typically used in European countries, while the DSM-IV-TR criteria are used in the United States and to varying degrees around the world, and are prevailing in research studies. The ICD-10 criteria put more emphasis on Schneiderian first-rank symptoms. In practice, agreement between the two systems is high.[74]
According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:[75]
- Characteristic symptoms: Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment).
- Delusions
- Hallucinations
- Disorganized speech, which is a manifestation of formal thought disorder
- Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- Negative symptoms: Blunted affect (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation)
- If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication.
- Social or occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Significant duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment).
If signs of disturbance are present for more than a month but less than six months, the diagnosis of schizophreniform disorder is applied.[75] Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, and various conditions may be classed as psychotic disorder not otherwise specified. Schizophrenia cannot be diagnosed if symptoms of mood disorder are substantially present (although schizoaffective disorder could be diagnosed), or if symptoms of pervasive developmental disorder are present unless prominent delusions or hallucinations are also present, or if the symptoms are the direct physiological result of a general medical condition or a substance, such as abuse of a drug or medication.
Subtypes
redigérThe DSM-IV-TR contains five sub-classifications of schizophrenia, although the developers of DSM-5 are recommending they be dropped from the new classification:[76][77]
- Paranoid type: Delusions or auditory hallucinations are present, but thought disorder, disorganized behavior, or affective flattening are not. Delusions are persecutory and/or grandiose, but in addition to these, other themes such as jealousy, religiosity, or somatization may also be present. (DSM code 295.3/ICD code F20.0)
- Disorganized type: Named hebephrenic schizophrenia in the ICD. Where thought disorder and flat affect are present together. (DSM code 295.1/ICD code F20.1)
- Catatonic type: The subject may be almost immobile or exhibit agitated, purposeless movement. Symptoms can include catatonic stupor and waxy flexibility. (DSM code 295.2/ICD code F20.2)
- Undifferentiated type: Psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met. (DSM code 295.9/ICD code F20.3)
- Residual type: Where positive symptoms are present at a low intensity only. (DSM code 295.6/ICD code F20.5)
The ICD-10 defines two additional subtypes:[77]
- Post-schizophrenic depression: A depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present. (ICD code F20.4)
- Simple schizophrenia: Insidious and progressive development of prominent negative symptoms with no history of psychotic episodes. (ICD code F20.6)
Differential
redigérPsychotic symptoms may be present in several other mental disorders, including bipolar disorder,[78] borderline personality disorder,[79] drug intoxication and drug-induced psychosis. Delusions ("non-bizarre") are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. Schizophrenia is comorbid with obsessive-compulsive disorder (OCD) considerably more often than could be explained by pure chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia.[80] A small number of people withdrawing from benzodiazepines experience a severe protracted withdrawal syndrome which can resemble schizophrenia and be misdiagnosed as such.[81]
A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms,[75] such as metabolic disturbance, systemic infection, syphilis, HIV infection, epilepsy, and brain lesions. Stroke, multiple sclerosis, hyperthyroidism, hypothyroidism and dementias such as Alzheimer's disease, Huntington's disease, frontotemporal dementia and Lewy Body dementia may also be associated with schizophrenia-like psychotic symptoms.[82] It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific medical indication or possible adverse effects from antipsychotic medication.
Prevention
redigérPrevention of schizophrenia is difficult as there are no reliable markers for the later development of the disease.[83] The evidence for the effectiveness of early interventions to prevent schizophrenia is inconclusive.[84] While there is some evidence that early intervention in those with a psychotic episode may improve short term outcomes, there is little benefit from these measures after five years.[2] Attempting to prevent schizophrenia in the prodrome phase is of uncertain benefit and therefore as of 2009 is not recommended.[85] Cognitive behavioral therapy may reduce the risk of psychosis in those at high risk after a year.[86] Another preventative measure is to avoid drugs that have been associated with development of the disorder, including cannabis, cocaine, and amphetamines.[3]
Management
redigérThe primary treatment of schizophrenia is antipsychotic medications, often in combination with psychological and social supports.[2] Hospitalization may occur for severe episodes either voluntarily or (if mental health legislation allows it) involuntarily. Long-term hospitalization is uncommon since deinstitutionalization beginning in the 1950s, although it still occurs.[5] Community support services including drop-in centers, visits by members of a community mental health team, supported employment[87] and support groups are common. Some evidence indicates that regular exercise has a positive effect on the physical and mental health of those with schizophrenia.[88]
Medication
redigérThe first-line psychiatric treatment for schizophrenia is antipsychotic medication,[89] which can reduce the positive symptoms of psychosis in about 7–14 days. Antipsychotics, however, fail to significantly ameliorate the negative symptoms and cognitive dysfunction.[23][90] In those on antipsychotics, continued use decreases the risk of relapse.[91][92] There is little evidence regarding consistent benefits from their use beyond two or three years.[92]
The choice of which antipsychotic to use is based on benefits, risks, and costs.[2] It is debatable whether, as a class, typical or atypical antipsychotics are better.[93][94] Both have equal drop-out and symptom relapse rates when typicals are used at low to moderate dosages.[95] There is a good response in 40–50%, a partial response in 30–40%, and treatment resistance (failure of symptoms to respond satisfactorily after six weeks to two or three different antipsychotics) in 20% of people.[23] Clozapine is an effective treatment for those who respond poorly to other drugs ("treatment-resistant" or "refractory" schizophrenia),[96] but it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in less than 4% of patients.[2][3][97]
With respect to side effects typical antipsychotics are associated with a higher rate of extrapyramidal side effects while atypicals are associated with considerable weight gain, diabetes and risk of metabolic syndrome.[95] While atypicals have fewer extrapyramidal side effects these differences are modest.[98] Some atypicals such as quetiapine and risperidone are associated with a higher risk of death compared to the typical antipsychotic perphenazine, while clozapine is associated with the lowest risk of death.[99] It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome, a rare but serious neurological disorder.[100]
For people who are unwilling or unable to take medication regularly, long-acting depot preparations of antipsychotics may be used to achieve control.[101] They reduce the risk of relapse to a greater degree than oral medications.[91] When used in combination with psychosocial interventions they may improve long-term adherence to treatment.[101] The American Psychiatric Association suggests considering stopping antipsychotics in some people if there are no symptoms for more than a year.[92]
Psychosocial
redigérA number of psychosocial interventions may be useful in the treatment of schizophrenia including: family therapy,[102] assertive community treatment, supported employment, cognitive remediation,[103] skills training, cognitive behavioral therapy (CBT), token economic interventions, and psychosocial interventions for substance use and weight management.[104] Family therapy or education, which addresses the whole family system of an individual, may reduce relapses and hospitalizations.[102] The evidence for CBT's effectiveness in either reducing symptoms or preventing relapse is minimal.[105][106] Art or drama therapy have not been well-researched.[107][108]
Prognosis
redigérSchizophrenia has great human and economic costs.[2] It results in a decreased life expectancy of 12–15 years, primarily because of its association with obesity, sedentary lifestyles, and smoking, with an increased rate of suicide playing a lesser role.[2] These differences in life expectancy increased between the 1970s and 1990s,[109] and between the 1990s and first decade of the 21st century did not change substantially in a health system with open access to care (Finland).[99]
Schizophrenia is a major cause of disability, with active psychosis ranked as the third-most-disabling condition after quadriplegia and dementia and ahead of paraplegia and blindness.[110] Approximately three-fourths of people with schizophrenia have ongoing disability with relapses[23] and 16.7 million people globally are deemed to have moderate or severe disability from the condition.[111] Some people do recover completely and others function well in society.[112] Most people with schizophrenia live independently with community support.[2] In people with a first episode of psychosis a good long-term outcome occurs in 42%, an intermediate outcome in 35% and a poor outcome in 27%.[113] Outcomes for schizophrenia appear better in the developing than the developed world.[114] These conclusions, however, have been questioned.[115][116]
There is a higher than average suicide rate associated with schizophrenia. This has been cited at 10%, but a more recent analysis of studies and statistics revises the estimate to 4.9%, most often occurring in the period following onset or first hospital admission.[7][117] Several times more (20 to 40%) attempt suicide at least once.[118][119] There are a variety of risk factors, including male gender, depression, and a high intelligence quotient.[118]
Schizophrenia and smoking have shown a strong association in studies world-wide.[120][121] Use of cigarettes is especially high in individuals diagnosed with schizophrenia, with estimates ranging from 80% to 90% being regular smokers, as compared to 20% of the general population.[121] Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content.[119] Some evidence suggests that paranoid schizophrenia may have a better prospect than other types of schizophrenia for independent living and occupational functioning.[122]
Epidemiology
redigér no data ≤ 185 185–197 197–207 207–218 218–229 229–240 | 240–251 251–262 262–273 273–284 284–295 ≥ 295 |
Schizophrenia affects around 0.3–0.7% of people at some point in their life,[2] or 24 million people worldwide as of 2011.[123] It occurs 1.4 times more frequently in males than females and typically appears earlier in men[3]—the peak ages of onset are 20–28 years for males and 26–32 years for females.[124] Onset in childhood is much rarer,[125] as is onset in middle- or old age.[126] Despite the received wisdom that schizophrenia occurs at similar rates worldwide, its prevalence varies across the world,[127] within countries,[128] and at the local and neighborhood level.[129] It causes approximately 1% of worldwide disability adjusted life years.[3] The rate of schizophrenia varies up to threefold depending on how it is defined.[2]
In 2000, the World Health Organization found the prevalence and incidence of schizophrenia to be roughly similar around the world, with age-standardized prevalence per 100,000 ranging from 343 in Africa to 544 in Japan and Oceania for men and from 378 in Africa to 527 in Southeastern Europe for women.[130]
History
redigérThe history of schizophrenia is complex and does not lend itself easily to a linear narrative.[131] Accounts of a schizophrenia-like syndrome are thought to be rare in the historical record before the 19th century, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning James Tilly Matthews, and accounts by Phillipe Pinel published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature.[132] The Latinized term dementia praecox was first used by German alienist Heinrich Schule in 1886 and then in 1891 by Arnold Pick in a case report of a psychotic disorder (hebephrenia). In 1893 Emil Kraepelin borrowed the term from Schule and Pick and in 1899 introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression).[133] Kraepelin believed that dementia praecox was probably caused by a long-term, smouldering systemic or "whole body" disease process that affected many organs and peripheral nerves in the body but which affected the brain after puberty in a final decisive cascade.[134] His use of the term dementia distinguished it from other forms of dementia such as Alzheimer's disease which typically occur later in life.[135] It is sometimes argued that the use of the term démence précoce in 1852 by the French physician Bénédict Morel constitutes the medical discovery of schizophrenia. However this account ignores the fact that there is little to connect Morel's descriptive use of the term and the independent development of the dementia praecox disease concept at the end of the nineteenth-century.[136]
The word schizophrenia—which translates roughly as "splitting of the mind" and comes from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind")[137]—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. American and British interpretations of Beuler led to the claim that he described its main symptoms as 4 A's: flattened Affect, Autism, impaired Association of ideas and Ambivalence.[138][139] Bleuler realized that the illness was not a dementia, as some of his patients improved rather than deteriorated, and thus proposed the term schizophrenia instead. Treatment was revolutionized in the mid-1950s with the development and introduction of chlorpromazine.[140]
In the early 1970s, the diagnostic criteria for schizophrenia were the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe.[141] This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. David Rosenhan's 1972 study, published in the journal Science under the title "On being sane in insane places", concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable.[142] These were some of the factors leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III in 1980.[143] The term schizophrenia is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. The confusion arises in part due to the literal interpretation of Bleuler's term schizophrenia (Bleuler originally associated Schizophrenia with dissociation and included split personality in his category of Schizophrenia[144][145]). Dissociative identity disorder (having a "split personality") was also often misdiagnosed as Schizophrenia based on the loose criteria in the DSM-II.[145][146] The first known misuse of the term to mean "split personality" was in an article by the poet T. S. Eliot in 1933.[147] Other scholars have traced earlier roots.[148]
Society and culture
redigérIn 2002 the term for schizophrenia in Japan was changed from Seishin-Bunretsu-Byō 精神分裂病 (mind-split-disease) to Tōgō-shitchō-shō 統合失調症 (integration disorder) to reduce stigma.[149] The new name was inspired by the biopsychosocial model; it increased the percentage of patients who were informed of the diagnosis from 37% to 70% over three years.[150]
In the United States, the cost of schizophrenia—including direct costs (outpatient, inpatient, drugs, and long-term care) and non-health care costs (law enforcement, reduced workplace productivity, and unemployment)—was estimated to be $62.7 billion in 2002.[151] The book and film A Beautiful Mind chronicles the life of John Forbes Nash, a Nobel Prize-winning mathematician who was diagnosed with schizophrenia.
Violence
redigérIndividuals with severe mental illness including schizophrenia are at a significantly greater risk of being victims of both violent and non-violent crime.[152] On the other hand, schizophrenia has sometimes been associated with a higher rate of violent acts, although this is primarily due to higher rates of drug use.[153] Rates of homicide linked to psychosis are similar to those linked to substance misuse, and parallel the overall rate in a region.[154] What role schizophrenia has on violence independent of drug misuse is controversial, but certain aspects of individual histories or mental states may be factors.[155]
Media coverage relating to schizophrenia tends to revolve around rare but unusual acts of violence. Furthermore, in a large, representative sample from a 1999 study, 12.8% of Americans believed that individuals with schizophrenia were "very likely" to do something violent against others, and 48.1% said that they were "somewhat likely" to. Over 74% said that people with schizophrenia were either "not very able" or "not able at all" to make decisions concerning their treatment, and 70.2% said the same of money management decisions.[156] The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.[157]
See also
redigérReferencer
redigérLitteratur
redigér- Cullberg, Johan (1999). Dynamisk Psykiatri. København: Hans Reitzels Forlag. ISBN 87-412-3092-2.
- Kasper, Siegfried (2009). Schizophrenia. United Kingdom: Informa Healthcare. s. 377. ISBN 13: 978-1-4200-8004-9.
{{cite book}}:|access-date=kræver at|url=også er angivet (hjælp); Tjek|isbn=: invalid character (hjælp); Tjek datoværdier i:|accessdate=(hjælp); Ukendt parameter|coauthors=ignoreret (|author=foreslået) (hjælp)
- Rosenberg, Raben (2009). FADL's forlag Klinisk neuropsykiatri - Fra molekyle til sygdom. København: FADL's forlag. ISBN 87-7749-414-8. Hentet 16/7-2013.
{{cite book}}: Tjek|url=(hjælp); Tjek datoværdier i:|accessdate=(hjælp); Ukendt parameter|coauthors=ignoreret (|author=foreslået) (hjælp)
Eksterne henvisninger
redigérFodnoter
redigér- ^ "Schizophrenia" Concise Medical Dictionary. Oxford University Press, 2010. Oxford Reference Online. Maastricht University Library. 29 June 2010 prepaid subscription only
- ^ a b c d e f g h i j k l m n o p q r s t van Os J, Kapur S (2009). "Schizophrenia" (PDF). Lancet. 374 (9690): 635-45. doi:10.1016/S0140-6736(09)60995-8. PMID 19700006.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp) - ^ a b c d e f g h i j k l Picchioni MM, Murray RM (2007). "Schizophrenia". BMJ. 335 (7610): 91-5. doi:10.1136/bmj.39227.616447.BE. PMC 1914490. PMID 17626963.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp) - ^ Baucum, Don (2006). Psychology (2nd ed. udgave). Hauppauge, N.Y.: Barron's. s. 182. ISBN 9780764134210.
{{cite book}}:|edition=har ekstra tekst (hjælp) - ^ a b Becker T, Kilian R (2006). "Psychiatric services for people with severe mental illness across western Europe: what can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?". Acta Psychiatrica Scandinavica Supplement. 113 (429): 9-16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476.
- ^ Buckley PF, Miller BJ, Lehrer DS, Castle DJ (2009). "Psychiatric comorbidities and schizophrenia". Schizophr Bull. 35 (2): 383-402. doi:10.1093/schbul/sbn135. PMC 2659306. PMID 19011234.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ a b Hor, K (2010 Nov). "Suicide and schizophrenia: a systematic review of rates and risk factors". Journal of psychopharmacology (Oxford, England). 24 (4 Suppl): 81-90. PMID 20923923.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp); Ukendt parameter|coauthors=ignoreret (|author=foreslået) (hjælp) - ^ a b Sundhedguiden.dk: Skizofreni. Besøgt d. 14/7 2013
- ^ Cullberg 1999 s. 263
- ^ Kasper 2009 s. 159
- ^ Hirsch SR; WeinbergerDR (2003). Schizophrenia. Wiley-Blackwell. s. 481. ISBN 978-0-632-06388-8.
- ^ a b c Carson VB (2000). Mental health nursing: the nurse-patient journey W.B. Saunders. ISBN 978-0-7216-8053-8. p. 638.
- ^ Hirsch SR; Weinberger DR (2003). Schizophrenia. Wiley-Blackwell. s. 21. ISBN 978-0-632-06388-8.
- ^ Baier, M (2010 Aug). "Insight in schizophrenia: a review". Current psychiatry reports. 12 (4): 356-61. PMID 20526897.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp) - ^ Ungvari GS, Caroff SN, Gerevich J (2010). "The catatonia conundrum: evidence of psychomotor phenomena as a symptom dimension in psychotic disorders". Schizophr Bull. 36 (2): 231-8. doi:10.1093/schbul/sbp105. PMID 19776208.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Schneider, K (1959). Clinical Psychopathology (5 udgave). New York: Grune & Stratton.
- ^ Nordgaard J, Arnfred SM, Handest P, Parnas J (2008). "The diagnostic status of first-rank symptoms". Schizophrenia Bulletin. 34 (1): 137-54. doi:10.1093/schbul/sbm044. PMC 2632385. PMID 17562695.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Sims A (2002). Symptoms in the mind: an introduction to descriptive psychopathology. Philadelphia: W. B. Saunders. ISBN 0-7020-2627-1.
- ^ Kneisl C. and Trigoboff E.(2009). Contemporary Psychiatric- Mental Health Nursing. 2nd edition. London: Pearson Prentice Ltd. p. 371
- ^ a b American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. ISBN 978-0-89042-025-6. p. 299
- ^ Rosenberg s. 239
- ^ Velligan DI and Alphs LD (marts 1, 2008). "Negative Symptoms in Schizophrenia: The Importance of Identification and Treatment". Psychiatric Times. 25 (3).
{{cite journal}}: CS1-vedligeholdelse: Dato automatisk oversat (link) - ^ a b c d Smith T, Weston C, Lieberman J (2010). "Schizophrenia (maintenance treatment)". Am Fam Physician. 82 (4): 338-9. PMID 20704164.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) Fodnotefejl: Ugyldigt<ref>tag; navnet "AFP10" er defineret flere gange med forskelligt indhold - ^ a b Addington J, Cadenhead KS, Cannon TD; et al. (2007). "North American prodrome longitudinal study: a collaborative multisite approach to prodromal schizophrenia research". Schizophrenia Bulletin. 33 (3): 665-72. doi:10.1093/schbul/sbl075. PMC 2526151. PMID 17255119.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Cullen KR, Kumra S, Regan J; et al. (2008). "Atypical Antipsychotics for Treatment of Schizophrenia Spectrum Disorders". Psychiatric Times. 25 (3).
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Amminger GP, Leicester S, Yung AR; et al. (2006). "Early onset of symptoms predicts conversion to non-affective psychosis in ultra-high risk individuals". Schizophrenia Research. 84 (1): 67-76. doi:10.1016/j.schres.2006.02.018. PMID 16677803.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Parnas J, Jorgensen A (1989). "Pre-morbid psychopathology in schizophrenia spectrum". British Journal of Psychiatry. 115: 623-7. PMID 2611591.
- ^ Coyle, Joseph (2006). "Chapter 54: The Neurochemistry of Schizophrenia". I Siegal, George J; Albers, R. Wayne; Brady, Scott T; Price, Donald (red.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects (Textbook) (7th udgave). Burlington, MA: Elsevier Academic Press. s. 876. ISBN 0-12-088397-X.
{{cite book}}:|format=kræver at|url=også er angivet (hjælp); Ugyldig|ref=harv(hjælp) - ^ Drake RJ, Lewis SW. Early detection of schizophrenia. Current Opinion in Psychiatry. 2005;18(2):147–50. doi:10.1097/00001504-200503000-00007. PMID 16639167.
- ^ a b Rosenberg s. 243
- ^ O'Donovan MC, Williams NM, Owen MJ (2003). "Recent advances in the genetics of schizophrenia". Hum. Mol. Genet. 12 Spec No 2: R125-33. doi:10.1093/hmg/ddg302. PMID 12952866.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ a b c Kasper et al. s. 78
- ^ Schacter, Daniel L. (2011). Psychology Ed. 2. 41 Madison Avenue New York, NY 10010: Worth Publishers. s. 578. ISBN 1–4292–3719–8.
{{cite book}}: Tjek|isbn=: invalid character (hjælp)CS1-vedligeholdelse: location (link) - ^ Rosenberg s. 245
- ^ Rosenberg s. 246
- ^ Craddock N, Owen MJ (2010). "The Kraepelinian dichotomy - going, going... But still not gone". The British Journal of Psychiatry. 196: 92-95. doi:10.1192/bjp.bp.109.073429. PMC 2815936. PMID 20118450.
- ^ Crow TJ (2008). "The 'big bang' theory of the origin of psychosis and the faculty of language". Schizophrenia Research. 102 (1-3): 31-52. doi:10.1016/j.schres.2008.03.010. PMID 18502103.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp) - ^ Mueser KT, Jeste DV (2008). Clinical Handbook of Schizophrenia. New York: Guilford Press. s. 22-23. ISBN 1-59385-652-0.
- ^ Rosenberg s. 247
- ^ Selten JP, Cantor-Graae E, Kahn RS (2007). "Migration and schizophrenia". Current Opinion in Psychiatry. 20 (2): 111-115. doi:10.1097/YCO.0b013e328017f68e. PMID 17278906.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Larson, Michael (2006-03-30). "Alcohol-Related Psychosis". eMedicine. WebMD. Hentet september 27, 2006.
{{cite web}}: CS1-vedligeholdelse: Dato automatisk oversat (link) - ^ Sagud M, Mihaljević-Peles A, Mück-Seler D; et al. (2009). "Smoking and schizophrenia" (PDF). Psychiatr Danub. 21 (3): 371-5. PMID 19794359.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp); Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ a b Gregg L, Barrowclough C, Haddock G (2007). "Reasons for increased substance use in psychosis". Clin Psychol Rev. 27 (4): 494-510. doi:10.1016/j.cpr.2006.09.004. PMID 17240501.
{{cite journal}}: CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Large M, Sharma S, Compton MT, Slade T, Nielssen O (2011). "Cannabis use and earlier onset of psychosis: a systematic meta-analysis". Arch. Gen. Psychiatry. 68 (6): 555-61. doi:10.1001/archgenpsychiatry.2011.5. PMID 21300939.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Leweke FM, Koethe D (2008). "Cannabis and psychiatric disorders: it is not only addiction". Addict Biol. 13 (2): 264-75. doi:10.1111/j.1369-1600.2008.00106.x. PMID 18482435.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp) - ^ Alcohol-Related Psychosis på eMedicine
- ^ Moore THM, Zammit S, Lingford-Hughes A; et al. (2007). "Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review". Lancet. 370 (9584): 319-328. doi:10.1016/S0140-6736(07)61162-3. PMID 17662880.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Sewell RA, Ranganathan M, D'Souza DC (2009 Apr). "Cannabinoids and psychosis". International review of psychiatry (Abingdon, England). 21 (2): 152-62. doi:10.1080/09540260902782802. PMID 19367509.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ McLaren JA, Silins E, Hutchinson D, Mattick RP, Hall W (2010). "Assessing evidence for a causal link between cannabis and psychosis: a review of cohort studies". Int. J. Drug Policy. 21 (1): 10-9. doi:10.1016/j.drugpo.2009.09.001. PMID 19783132.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Ben Amar M, Potvin S (2007 Jun). "Cannabis and psychosis: what is the link?". Journal of Psychoactive Drugs. 39 (2): 131-42. doi:10.1080/02791072.2007.10399871. PMID 17703707.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp) - ^ E. S. Susser, S. P. Lin, "Schizophrenia after prenatal exposure to the Dutch Hunger Winter of 1944-1945", Archives of General Psychiatry, 2004. Engelsk-sproget videnskabelig artikel om skizofreni og sultkatastrofen i Holland.
- ^ Rosenberg s. 248
- ^ a b Rosenberg s. 242
- ^ Broome MR, Woolley JB, Tabraham P; et al. (2005). "What causes the onset of psychosis?". Schizophr. Res. 79 (1): 23-34. doi:10.1016/j.schres.2005.02.007. PMID 16198238.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp); Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Bentall RP, Fernyhough C, Morrison AP, Lewis S, Corcoran R (2007). "Prospects for a cognitive-developmental account of psychotic experiences". Br J Clin Psychol. 46 (Pt 2): 155-73. doi:10.1348/014466506X123011. PMID 17524210.
{{cite journal}}: CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Kurtz MM (2005). "Neurocognitive impairment across the lifespan in schizophrenia: an update". Schizophrenia Research. 74 (1): 15-26. doi:10.1016/j.schres.2004.07.005. PMID 15694750.
- ^ Cohen AS, Docherty NM (2004). "Affective reactivity of speech and emotional experience in patients with schizophrenia". Schizophrenia Research. 69 (1): 7-14. doi:10.1016/S0920-9964(03)00069-0. PMID 15145465.
- ^ Horan WP, Blanchard JJ (2003). "Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping". Schizophrenia Research. 60 (2-3): 271-83. doi:10.1016/S0920-9964(02)00227-X. PMID 12591589.
- ^ Smith B, Fowler DG, Freeman D; et al. (2006). "Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations". Schizophr. Res. 86 (1-3): 181-8. doi:10.1016/j.schres.2006.06.018. PMID 16857346.
{{cite journal}}: Eksplicit brug af et al. i:|author=(hjælp); Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Beck, AT (2004). "A Cognitive Model of Schizophrenia". Journal of Cognitive Psychotherapy. 18 (3): 281-88. doi:10.1891/jcop.18.3.281.65649.
- ^ Bell V, Halligan PW, Ellis HD (2006). "Explaining delusions: a cognitive perspective". Trends in Cognitive Science. 10 (5): 219-26. doi:10.1016/j.tics.2006.03.004. PMID 16600666.
{{cite journal}}: CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE, Dunn G. Acting on persecutory delusions: the importance of safety seeking. Behav Res Ther. 2007;45(1):89–99. doi:10.1016/j.brat.2006.01.014. PMID 16530161.
- ^ Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P (2006). "Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms". Schizophr Bull. 32 Suppl 1: S24-31. doi:10.1093/schbul/sbl014. PMC 2632539. PMID 16885206.
{{cite journal}}: Ukendt parameter|month=ignoreret (hjælp)CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Kircher, Tilo and Renate Thienel. The Boundaries of Consciousness. Amsterdam: Elsevier; 2006. ISBN 0-444-52876-8. Functional brain imaging of symptoms and cognition in schizophrenia. s. 302.
- ^ Coyle 2006, s. 878
- ^ Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. Journal of Clinical Psychiatry. 2006;67(Suppl 9):3–8. PMID 16965182.
- ^ Insel TR. Rethinking schizophrenia. Nature. 2010;468(7321):187–93. doi:10.1038/nature09552. PMID 21068826.
- ^ Laruelle M, Abi-Dargham A, van Dyck CH, et al.. Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc. Natl. Acad. Sci. U.S.A.. 1996;93(17):9235–40. doi:10.1073/pnas.93.17.9235. PMID 8799184.
- ^ Jones HM, Pilowsky LS. Dopamine and antipsychotic drug action revisited. British Journal of Psychiatry. 2002;181:271–275. doi:10.1192/bjp.181.4.271. PMID 12356650.
- ^ Konradi C, Heckers S. Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics. 2003;97(2):153–79. doi:10.1016/S0163-7258(02)00328-5. PMID 12559388.
- ^ Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA. Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology. 2001;25(4):455–67. doi:10.1016/S0893-133X(01)00243-3. PMID 11557159.
- ^ Coyle JT, Tsai G, Goff D. Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences. 2003;1003:318–27. doi:10.1196/annals.1300.020. PMID 14684455.
- ^ Tuominen HJ, Tiihonen J, Wahlbeck K. Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2005;72(2–3):225–34. doi:10.1016/j.schres.2004.05.005. PMID 15560967.
- ^ Jakobsen KD, Frederiksen JN, Hansen T, et al.. Reliability of clinical ICD-10 schizophrenia diagnoses. Nordic Journal of Psychiatry. 2005;59(3):209–12. doi:10.1080/08039480510027698. PMID 16195122.
- ^ a b c American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Publishing, Inc.; 2000 [Hentet 2008-07-04]. ISBN 0-89042-024-6. Schizophrenia.
- ^ American Psychiatric Association DSM-5 Work Groups (2010) Proposed Revisions – Schizophrenia and Other Psychotic Disorders. Retrieved 17 February 2010.
- ^ a b The ICD-10 Classification of Mental and Behavioural Disorders [pdf]; p. 26.
- ^ Pope HG. Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports. Hospital and Community Psychiatry. 1983 [Hentet 2008-02-24];34:322–28.
- ^ McGlashan TH. Testing DSM-III symptom criteria for schizotypal and borderline personality disorders. Archives of General Psychiatry. 1987;44(2):143–8. PMID 3813809.
- ^ Bottas A. Comorbidity: Schizophrenia With Obsessive-Compulsive Disorder. Psychiatric Times. April 15, 2009;26(4).
- ^ Gabbard, Glen O. (15 maj 2007). Gabbard's Treatments of Psychiatric Disorders, Fourth Edition (Treatments of Psychiatric Disorders). American Psychiatric Publishing. s. 209-211. ISBN 1-58562-216-8.
{{cite book}}: CS1-vedligeholdelse: Dato automatisk oversat (link) - ^ Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". I Bradley WG, Daroff RB, Fenichel GM, Jankovic J (red.). Bradley's neurology in clinical practice. Vol. 1 (6th udgave). Philadelphia, PA: Elsevier/Saunders. s. 92-111. ISBN 1-4377-0434-4.
{{cite book}}: CS1-vedligeholdelse: Flere navne: authors list (link) - ^ Cannon TD, Cornblatt B, McGorry P. The empirical status of the ultra high-risk (prodromal) research paradigm. Schizophrenia Bulletin. 2007;33(3):661–4. doi:10.1093/schbul/sbm031. PMID 17470445.
- ^ Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev. 2006;(4):CD004718. doi:10.1002/14651858.CD004718.pub2. PMID 17054213.
- ^ de Koning MB, Bloemen OJ, van Amelsvoort TA, et al.. Early intervention in patients at ultra high risk of psychosis: benefits and risks. Acta Psychiatr Scand. 2009;119(6):426–42. doi:10.1111/j.1600-0447.2009.01372.x. PMID 19392813.
- ^ Stafford, MR (2013 Jan 18). "Early interventions to prevent psychosis: systematic review and meta-analysis". BMJ (Clinical research ed.). 346: f185. PMID 23335473.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp); Ukendt parameter|coauthors=ignoreret (|author=foreslået) (hjælp) - ^ McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A. Cognitive training for supported employment: 2–3 year outcomes of a randomized controlled trial.. American Journal of Psychiatry. 2007;164(3):437–41. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- ^ Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010;(5):CD004412. doi:10.1002/14651858.CD004412.pub2. PMID 20464730.
- ^ National Collaborating Centre for Mental Health. Gaskell and the British Psychological Society. Schizophrenia: Full national clinical guideline on core interventions in primary and secondary care [PDF]; 2009-03-25 [Hentet 2009-11-25].
- ^ Tandon R, Keshavan MS, Nasrallah HA. Schizophrenia, "Just the Facts": what we know in 2008 part 1: overview. Schizophrenia Research. 2008;100(1–3):4–19. doi:10.1016/j.schres.2008.01.022. PMID 18291627.
- ^ a b Leucht S, Tardy M, Komossa K, et al.. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–71. doi:10.1016/S0140-6736(12)60239-6. PMID 22560607.
- ^ a b c Harrow, M (2013 Mar 19). "Does Long-Term Treatment of Schizophrenia With Antipsychotic Medications Facilitate Recovery?". Schizophrenia bulletin. PMID 23512950.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp); Ukendt parameter|coauthors=ignoreret (|author=foreslået) (hjælp) - ^ Kane JM, Correll CU. Pharmacologic treatment of schizophrenia. Dialogues Clin Neurosci. 2010;12(3):345–57. PMID 20954430.
- ^ Antipsychotics in Adults With Schizophrenia: Comparative Effectiveness of First-Generation Versus Second-Generation Medications: A Systematic Review and Meta-analysis.. Annals of internal medicine. 2012 Aug 14. PMID 22893011.
- ^ a b Schultz SH, North SW, Shields CG. Schizophrenia: a review. Am Fam Physician. 2007;75(12):1821–9. PMID 17619525.
- ^ Taylor DM. Refractory schizophrenia and atypical antipsychotics. J Psychopharmacol. 2000;14(4):409-418. doi:10.1177/026988110001400411.
- ^ Essali A, Al-Haj Haasan N, Li C, Rathbone J. Clozapine versus typical neuroleptic medication for schizophrenia. Cochrane Database Syst Rev. 2009;(1):CD000059. doi:10.1002/14651858.CD000059.pub2. PMID 19160174.
- ^ Tandon R, Belmaker RH, Gattaz WF, et al.. World Psychiatric Association Pharmacopsychiatry Section statement on comparative effectiveness of antipsychotics in the treatment of schizophrenia. Schizophr. Res.. 2008;100(1–3):20–38. doi:10.1016/j.schres.2007.11.033. PMID 18243663.
- ^ a b Chwastiak LA, Tek C. The unchanging mortality gap for people with schizophrenia. Lancet. 2009;374(9690):590–2. doi:10.1016/S0140-6736(09)61072-2. PMID 19595448.
- ^ Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T. Neuroleptic malignant syndrome and atypical antipsychotic drugs. Journal of Clinical Psychiatry. 2004;65(4):464–70. doi:10.4088/JCP.v65n0403. PMID 15119907.
- ^ a b McEvoy JP. Risks versus benefits of different types of long-acting injectable antipsychotics. J Clin Psychiatry. 2006;67 Suppl 5:15–8. PMID 16822092.
- ^ a b Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2010;12:CD000088. doi:10.1002/14651858.CD000088.pub3. PMID 21154340.
- ^ Medalia A, Choi J. Cognitive remediation in schizophrenia.. Neuropsychology Rev. 2009;19(3):353–364. doi:10.1007/s11065-009-9097-y. PMID 19444614.
- ^ Dixon LB, Dickerson F, Bellack AS, et al.. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):48–70. doi:10.1093/schbul/sbp115. PMID 19955389.
- ^ Lynch D, Laws KR, McKenna PJ. Cognitive behavioural therapy for major psychiatric disorder: does it really work? A meta-analytical review of well-controlled trials. Psychol Med. 2010;40(1):9–24. doi:10.1017/S003329170900590X. PMID 19476688.
- ^ Jones C, Cormac I, Silveira da Mota Neto JI, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database Syst Rev. 2004;(4):CD000524. doi:10.1002/14651858.CD000524.pub2. PMID 15495000.
- ^ Ruddy R, Milnes D. Art therapy for schizophrenia or schizophrenia-like illnesses.. Cochrane Database Syst Rev. 2005;(4):CD003728. doi:10.1002/14651858.CD003728.pub2. PMID 16235338.
- ^ Ruddy RA, Dent-Brown K. Drama therapy for schizophrenia or schizophrenia-like illnesses.. Cochrane Database Syst Rev. 2007;(1):CD005378. doi:10.1002/14651858.CD005378.pub2. PMID 17253555.
- ^ Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time?. Arch. Gen. Psychiatry. 2007;64(10):1123–31. doi:10.1001/archpsyc.64.10.1123. PMID 17909124.
- ^ Ustun TB. Multiple-informant ranking of the disabling effects of different health conditions in 14 countries. The Lancet. 1999;354(9173):111–15. doi:10.1016/S0140-6736(98)07507-2. PMID 10408486.
- ^ The global burden of disease : 2004 update.. [Online-Ausg.] ed. Geneva, Switzerland: World Health Organization; 2008. ISBN 9789241563710. s. 35.
- ^ Warner R. Recovery from schizophrenia and the recovery model. Curr Opin Psychiatry. 2009;22(4):374–80. doi:10.1097/YCO.0b013e32832c920b. PMID 19417668.
- ^ Menezes NM, Arenovich T, Zipursky RB. A systematic review of longitudinal outcome studies of first-episode psychosis. Psychol Med. 2006;36(10):1349–62. doi:10.1017/S0033291706007951. PMID 16756689.
- ^ Isaac M, Chand P, Murthy P. Schizophrenia outcome measures in the wider international community. Br J Psychiatry Suppl. 2007;50:s71–7. PMID 18019048.
- ^ Cohen A, Patel V, Thara R, Gureje O. Questioning an axiom: better prognosis for schizophrenia in the developing world?. Schizophr Bull. 2008;34(2):229–44. doi:10.1093/schbul/sbm105. PMID 17905787.
- ^ Burns J. Dispelling a myth: developing world poverty, inequality, violence and social fragmentation are not good for outcome in schizophrenia. Afr J Psychiatry (Johannesbg). 2009;12(3):200–5. PMID 19894340.
- ^ Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Archives of General Psychiatry. 2005;62(3):247–53. doi:10.1001/archpsyc.62.3.247. PMID 15753237.
- ^ a b Carlborg A, Winnerbäck K, Jönsson EG, Jokinen J, Nordström P. Suicide in schizophrenia. Expert Rev Neurother. 2010;10(7):1153–64. doi:10.1586/ern.10.82. PMID 20586695.
- ^ a b American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. ISBN 978-0-89042-025-6. p. 304
- ^ De Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophrenia research. 2005;76(2-3):135–57. doi:10.1016/j.schres.2005.02.010. PMID 15949648.
- ^ a b Keltner NL, Grant JS. Smoke, Smoke, Smoke That Cigarette. Perspectives in Psychiatric Care. 2006;42(4):256. doi:10.1111/j.1744-6163.2006.00085.x. PMID 17107571.
- ^ American Psychiatric Association. Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Pub. ISBN 978-0-89042-025-6. p. 314
- ^ World Health Organization. Schizophrenia; 2011 [Hentet February 27, 2011].
- ^ Castle D, Wessely S, Der G, Murray RM. The incidence of operationally defined schizophrenia in Camberwell, 1965–84. The British Journal of Psychiatry. 1991;159:790–4. doi:10.1192/bjp.159.6.790. PMID 1790446.
- ^ Kumra S, Shaw M, Merka P, Nakayama E, Augustin R. Childhood-onset schizophrenia: research update. Canadian Journal of Psychiatry. 2001;46(10):923–30. PMID 11816313.
- ^ Hassett Anne, et al. (eds). Psychosis in the Elderly. London: Taylor and Francis.; 2005. ISBN 1-84184-394-6. s. 6.
- ^ Jablensky A, Sartorius N, Ernberg G, et al.. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychological Medicine Monograph Supplement. 1992;20:1–97. doi:10.1017/S0264180100000904. PMID 1565705.
- ^ Kirkbride JB, Fearon P, Morgan C, et al.. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study. Archives of General Psychiatry. 2006;63(3):250–8. doi:10.1001/archpsyc.63.3.250. PMID 16520429.
- ^ Kirkbride JB, Fearon P, Morgan C, et al.. Neighbourhood variation in the incidence of psychotic disorders in Southeast London. Social Psychiatry and Psychiatric Epidemiology. 2007;42(6):438–45. doi:10.1007/s00127-007-0193-0. PMID 17473901.
- ^ Ayuso-Mateos, Jose Luis. "Global burden of schizophrenia in the year 2000" (PDF). World Health Organization. Hentet februar 27, 2013.
{{cite web}}: CS1-vedligeholdelse: Dato automatisk oversat (link) - ^ Yuhas, Daisy. "Throughout History, Defining Schizophrenia Has Remained a Challenge". Scientific American Mind (March/April 2013). Hentet 3 marts 2013.
{{cite web}}: CS1-vedligeholdelse: Dato automatisk oversat (link) - ^ Heinrichs RW. Historical origins of schizophrenia: two early madmen and their illness. Journal of the History of the Behavioral Sciences. 2003;39(4):349–63. doi:10.1002/jhbs.10152. PMID 14601041.
- ^ Noll, Richard (2011). American Madness:The Rise and Fall of Dementia Praecox. Cambridge, MA: Harvard University Press. ISBN 978-0-674-04739-6.
- ^ Noll, Richard (2012). "Whole Body Madness". Psychiatric Times. 29 (12): 13-14.
- ^ Hansen RA, Atchison B. Conditions in occupational therapy: effect on occupational performance. Hagerstown, MD: Lippincott Williams & Wilkins; 2000. ISBN 0-683-30417-8.
- ^ Berrios G.E., Luque R, Villagran J. Schizophrenia: a conceptual history. International Journal of Psychology and Psychological Therapy. 2003;3(2):111–140.
- ^ Kuhn R. Eugen Bleuler's concepts of psychopathology. History of Psychiatry. 2004;15(3):361–6. doi:10.1177/0957154X04044603. PMID 15386868.
- ^ Stotz-Ingenlath G. Epistemological aspects of Eugen Bleuler's conception of schizophrenia in 1911 [PDF]. Medicine, Health Care and Philosophy. 2000;3(2):153–9. doi:10.1023/A:1009919309015. PMID 11079343.
- ^ McNally, Kiernan (2009). "Eugen Bleuler's "Four A's"". History of Psychology. 12: 43-59.
- ^ Turner T. Unlocking psychosis. British Medical Journal. 2007;334(suppl):s7. doi:10.1136/bmj.39034.609074.94. PMID 17204765.
- ^ Wing JK. International comparisons in the study of the functional psychoses. British Medical Bulletin. 1971;27(1):77–81. PMID 4926366.
- ^ Rosenhan D. On being sane in insane places. Science. 1973;179(4070):250–8. doi:10.1126/science.179.4070.250. PMID 4683124.
- ^ Wilson M. DSM-III and the transformation of American psychiatry: a history. American Journal of Psychiatry. 1993;150(3):399–410. PMID 8434655.
- ^ Stotz-Ingenlath G: Epistemological aspects of Eugen Bleuler’s conception of schizophrenia in 1911. Med Health Care Philos 2000; 3:153—159
- ^ a b Hayes, J. A., & Mitchell, J. C. (1994). Mental health professionals' skepticism about multiple personality disorder. Professional Psychology: Research and Practice, 25, 410-415
- ^ Putnam, Frank W. (1989). Diagnosis and Treatment of Multiple Personality Disorder. New York: The Guilford Press. pp. 351. ISBN 0-89862-177-1
- ^ Berrios, G. E.; Porter, Roy. A history of clinical psychiatry: the origin and history of psychiatric disorders. London: Athlone Press; 1995. ISBN 0-485-24211-7.
- ^ McNally, K (2007 Winter). "Schizophrenia as split personality/Jekyll and Hyde: the origins of the informal usage in the English language". Journal of the history of the behavioral sciences. 43 (1): 69-79. PMID 17205539.
{{cite journal}}: Tjek datoværdier i:|date=(hjælp) - ^ Kim Y, Berrios GE. Impact of the term schizophrenia on the culture of ideograph: the Japanese experience. Schizophr Bull. 2001;27(2):181–5. PMID 11354585.
- ^ Sato M. Renaming schizophrenia: a Japanese perspective. World Psychiatry. 2004;5(1):53–55. PMID 16757998.
- ^ Wu EQ. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66(9):1122–9. PMID 16187769.
- ^ Maniglio R. Severe mental illness and criminal victimization: a systematic review. Acta Psychiatr Scand. 2009;119(3):180–91. doi:10.1111/j.1600-0447.2008.01300.x. PMID 19016668.
- ^ Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med.. 2009;6(8):e1000120. doi:10.1371/journal.pmed.1000120. PMID 19668362.
- ^ Large M, Smith G, Nielssen O. The relationship between the rate of homicide by those with schizophrenia and the overall homicide rate: a systematic review and meta-analysis. Schizophr. Res.. 2009;112(1-3):123–9. doi:10.1016/j.schres.2009.04.004. PMID 19457644.
- ^ Bo S, Abu-Akel A, Kongerslev M, Haahr UH, Simonsen E. Risk factors for violence among patients with schizophrenia. Clin Psychol Rev. 2011;31(5):711–26. doi:10.1016/j.cpr.2011.03.002. PMID 21497585.
- ^ Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health. 1999;89(9):1339–45. doi:10.2105/AJPH.89.9.1339. PMID 10474550.
- ^ Phelan JC, Link BG, Stueve A, Pescosolido BA. Public Conceptions of Mental Illness in 1950 and 1996: What Is Mental Illness and Is It to be Feared?. Journal of Health and Social Behavior. 2000;41(2):188–207. doi:10.2307/2676305.
External links
redigér- Christian89/Sandkasse2 på Curlie (som bygger videre på Open Directory Project)
Skabelon:Featured article Skabelon:Mental and behavioural disorders